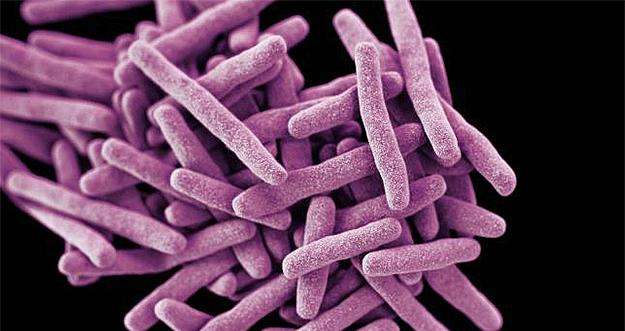
Candida auris (also referred to as C. auris), is a yeast-like fungus that has recently emerged as a worldwide invasive, multi-drug resistant pathogen. C. auris is not a health risk to the general public, but is a risk for patients who are already immunocompromised or critically ill. Some strains of C. auris are resistant to all drugs. C. auris can cause bloodstream, wound and ear infections.
What are the symptoms of C. auris infection?
Signs and symptoms of C. auris infection include:
- fever and chills while on antimicrobial medication
- sepsis
- isolation of Candida-like yeast from the patient’s blood, and
- little or no patient response or improvement with conventional antifungal therapy
How is C. auris infection diagnosed?
Because symptoms of C. auris are similar to other fungal infections and because C. auris is often misidentified as a number of different organisms when traditional testing is used, C. auris can be difficult to identify. All testing must be conducted in laboratories approved to conduct C. auris-specific tests. The NYS Department of Health’s Wadsworth Laboratory is the only lab that has been approved to conduct C. auris tests in NYS.
Who is at risk?
C. auris is an opportunistic infection that is typically acquired in a hospital setting. Those who are at highest risk of infection are patients who have been in the ICU for a long period of time or have a central venous catheter placed in a large vein and have previously received antibiotics or antifungal medications. At this time no healthcare workers treating infected patients have tested positive for C. auris.
How is C. auris spread?
C. auris is typically spread in hospital or long-term care settings through contact with contaminated surfaces or equipment or from physical contact with an infected person. C. auris is hardier than other candida species and, therefore, can survive longer on surfaces. There are currently no known cases of C. auris being spread through any mode of transmission other than contact.
What infection control measures are required?
In acute care settings, strict standard and universal precautions must be followed. Infected patients should, whenever possible, be isolated in a single patient room. Gowns and gloves should be worn and strict hand hygiene followed. If possible, equipment should be limited to the use of the infected patient and not shared with other patients. If equipment must be used on multiple patients, the NYS Department of Health recommends that the equipment be thoroughly disinfected with an EPA-approved hospital-grade cleaner that is effective against C. diff.
Nursing home residents should, whenever possible, be placed in a single-resident room and placed on contact precautions. Strict hand hygiene should be followed. The NYS Department of Health has not yet determined if a resident with C. auris infection must be restricted to his/her room and, if so, for how long a period.
The duration that infection control precautions must be followed is not yet known. It takes many patients months to clear the fungus from their system. At this time it is unclear how long these patients may be infectious to others.
How can C. auris infection be prevented?
Adherence to strict infection control protocols is key to limiting the risk of infection. Every healthcare facility should be reviewing its protocols to make sure they adequately address C. auris infection prevention. The NYS Department of Health will also assist healthcare facilities determine if infection control measures are adequate.
How dangerous is C. auris?
It is not currently known how much of the general public may carry the C. auris fungus. However, patients with lab-identified C. auris have a mortality rate of approximately 60%. These patients typically suffer from other serious co-morbidities, so it is difficult to determine if C. auris is the cause of death.
What steps is the NYS Department of Health taking to control the spread of C. auris?
The NYS Department of Health is closely surveilling cases of C. auris and taking the following steps to try to limit the infection’s spread:
- Meeting with stakeholders including infection control specialists, local departments of health, healthcare facility trade associations, healthcare worker unions and others to share information and solicit feedback
- Developing training for healthcare, transport and environmental services workers
- Conducting contact surveillance
- Developing a rapid test for faster identification of C. auris infection
- Developing a self-assessment tool for healthcare facilities to determine what additional measures need to be taken to properly identify, treat and control the spread of C. auris
- Conducting on-site audits of hospitals and long-term care facilities to assess infection control practices
- Developing ongoing guidance for hospitals, long-term care facilities and homecare based on newly emerging information related to treatment and infection control
- Requiring all sending facilities to contact receiving facilities by phone when a patient with C. auris infection is transferred and requiring that this information be displayed prominently on discharge or transfer documentation.
For more information contact the NYSNA Nursing Education and Practice department at 212-785-0157.
Sources: U.S. Centers for Disease Control, NYS Department of Health, World Health Organization