Public hearings critical to the future of special Medicaid funding in New York State — a total of $6.2 billion over five years — were held on February 17 in Albany. NYSNA was widely acknowledged to have played the central role in providing analysis and detail of the blueprint’s pros and cons.
DSRIP – the Delivery System Reform Incentive Payment Program — is in final stages of evaluating 25 Performing Provider Systems (PPS), a determination that will result in first stages of the distribution of funds. Evaluations will be ongoing during DSRIP’s term. Most of the PPS’s contain hospitals staffed by NYSNA members. This fact, as well as plans outlined in some of the PPS proposals that negatively impact RN scope of practice, were among criticisms referred to by NYSNA members in their testimonies.
Here are excerpts from a number of testimonies presented to DSRIP members:
|
NYSNA supports these goals of DSRIP: Quality care for Medicaid patients, better health outcomes, reduction of unnecessary hospital usage. We want to work on these goals; we want to be integral to this process — planning, participating and integrating in close collaboration with community leaders and groups at every stage, for real improvements for our patients. Inequality is the most compelling issue of our time. On that short list of terrible wrongs — healthcare disparities stand out. Ending healthcare disparities is NYSNA’s top priority. I regret that so little time has been committed to public comment on DSRIP, a major commitment of billions of dollars of public money in an area of such critical concern and need: meeting the healthcare needs of New Yorkers. Why so little outreach to the public over the last weeks and months, so little explanation and engagement? Transparency, public review and input, as put forward by CMS and New York State, were promised. I do not believe that promise has been kept. I would ask on behalf of NYSNA, our patients and the many public health advocates with whom we interact: more public comment is imperative. NYSNA is vigilant in the protection of our patients. We are prepared with other patient advocates, public health experts, other unions and community organizations to re-orient DSRIP away from those seeking to profit from it. A single payer system is very much on the agenda of many in our state- patients, legislators, city officials, unions, including NYSNA, consumer groups and public health experts. Its results are evidence-based, and in many countries single payer systems are achieving better healthcare outcomes, while demonstrating cost efficiency at the same time. This is consistent with the stated goals of DSRIP and should be high on this body’s agenda. Access to high quality care is grounded upon two principles: What is clinically appropriate and what is evidence-based. We are here, as nurses, to make certain that both of these principles are at work in the DSRIP process, to assure that all decisions have an empirical basis and that funds reach real need. It is well within our combined abilities – organizational and political – to make DSRIP work. To that end, nurses will monitor this process closely and intervene when necessary. It would appear that that necessity is upon us. – Judy Sheridan-Gonzalez, RN and President of the Board of Directors, NYSNA [Montefiore Hospital, Bronx] |
|
I have a great deal of experience working with at-risk populations, often dependent on Medicaid. Recently St. Elizabeth Medical Center acquired property in the town of New Hartford and moved a number of outpatient services there, such as X-rays, and outpatient lab work. However, following the expansion, access to these services at the main hospital of St. Elizabeth’s – where they had traditionally been available – became more difficult for inner city patients to access. – Ethel Mathis, RN, St. Elizabeth Medical Center, Utica [Central NY PPS] |
|
I want to take this opportunity before you today to focus on another dimension of this PPS application, for its implications to the nursing profession, to evidence-based standards, to professional disease management and better patient outcomes. I am talking about scope of practice. This has a basis in both the ethics of my profession and in the laws of the State of New York. In the details of this PPS there appears to be a very real prospect of a shift of care away from those with licensure to others whose skills and experience are not those of registered nurse. – Julie Semente, RN, worked as a nurse in Brooklyn for more than 30 years [Community of Care PPS] |
|
The Nassau Queens PPS is seeking exemptions or waivers on a range of practices, some related to restrictions on referrals and revenue sharing, others on licensing and co-locations for mental health and substance abuse services. These should be examined. – James Morgan, RN, Syosset Hospital, Syosset [Nassau Queens PPS] |
|
We very much want to play a meaningful role in the DSRIP process and share the goals of improved quality care for Medicaid patients, improving actual health outcomes and lowering costs of care per patient by reducing unnecessary hospital usage. – Anthony Ciampa, RN and Member, Board of Directors, NYSNA. New York Presbyterian Hospital, New York City. [New York and Presbyterian Hospital PPS] |
|
We support DSRIP and its stated goals and very much want to work with you to make sure that communities in need receive this critical funding. – Cecilia Jordan, RN and Director, NYSNA HHC/Mayorals |
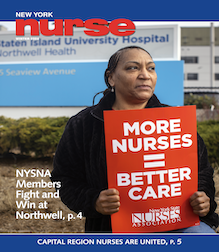
Additional testimony at the Feb. 17 DSRIP Hearings was provided by NYSNA Members (l to r, from top): Ethel Mathis, RN; Cecilia Jordan, RN; James Morgan, RN; Jayne Camissa, RN; Make Pattison, RN; and Mary Thompson, RN.
|
There are concerns that amidst… expansion Westchester Medical Center’s public mission may be diluted. The expansion was accomplished with little to no public input and DSRIP should scrutinize the PPS on these grounds. The PPS is seeking to waive Certificate of Need requests, including requests to decertify beds. At hospitals in Kingston and Port Jervis, under the Westchester umbrella, efforts are underway to decertify beds, which will have a significant impact on these communities. Major shifts in workforce are also proposed in the PPS. One-fifth of the staff in the PPS will be degraded, which can only undercut quality patient care. Scope of nursing practice issues are also implicated in the PPS, as there may be plans to have non-nurses carry out jobs that now belong to RNs. Eliminating RNs does away with professional care and has a profound impact on quality care. – Jayne Cammisa, RN, Westchester Medical Center, Valhalla [Westchester Medical Center PPS] |
|
As an ER nurse, I have a first-hand perspective on the entry point for healthcare services for many patients that are dependent upon Medicaid. Our ER is generally overflowing with patients in hallways, excessive wait times, and generally not enough nurses to always provide the proper timely care. On top of this, a large percentage of the patients are dependent upon Medicaid for accessing healthcare, yet the ER is still their entry point. Meanwhile, those who are in need of actual emergency care, have to contend with receiving care in this environment. Improvements are needed, clearly. Yet they must not come at the expense of our patients, or quality care delivered by trained RNs like myself. – Mike Pattison, RN, St. Elizabeth’s Medical Center, Utica [Mohawk Valley PPS and the Central NY PPS] |
|
I regularly see patients who are Medicaid dependent and still cannot afford all of their necessary medications. They tell me stories of having to make the hard decisions of buying medications or having to pay their rent. I have even seen patients whose failure to take their meds results in heart attacks or other serious conditions – resulting in unnecessary hospital admissions. Thus we very much welcome DSRIP and hope, with your attention and input from our communities, we can work together for more access to healthcare and better outcomes. The PPS failed to conduct a thorough or realistic analysis of the impact on employees who are to be redeployed or retrained, other than to offer an estimate that 55% of the workforce will need to be retrained. A fair amount of additional information, detail and focus is required to bring this application to completion. – Mary Thompson, RN, Utica [Mohawk Valley PPS] |