NYSNA nurses helped save the lives of 58,950 COVID-19 patients, according to the data of May 3, 2020. Against the odds, nurses persevered in very difficult conditions and, while the number of patients who died from the virus is substantial — 19,189 — many lives were saved, and the work of saving lives continues.
Community support is strong for Long Island nurses
NYSNA’s “Protect Our Direct Caregivers with Proper PPEs Vigil” took place at St. Catherine of Siena Medical Center in Smithtown on April 23, demanding more PPE and better staffing to slow the spread of COVID-19. The Long Island community came out to support them. Smithtown Supervisor Edward Wehrheim, Town Clerk Vincent Puleo, and leaders from the Nesconset Fire Department and Plumbers Local Union #200 all were there to show solidarity with the nurses. What’s more, the All Hands and Hearts organization, OK Petroleum, Smithtown Elected Officials, and the Rengel family took the opportunity to present frontline staff with substantial donation of PPE.
Sub-standard care guidelines
“We appreciate all the community support,” said Meg Comparato, RN. “In times like these, it has been so important to have union support standing with us. We as a society would never send our police and fire personnel to work without proper gear, why did the NYS DOH and our employer downgrade the guidelines so much as to put nurses in harm’s way?”
What Comparato, fellow nurses and public health experts have questioned is why the Centers for Disease Control set guidelines on a “crisis” level, allowing for re-use of N95s and allowing the New York State Department of Health to do the same. This resulted in sub-standard care guidelines.
“Coming to work should not be a scary thing,” said Tammy Miller, RN, Chair, NYSNA Executive Committee. “Reusing masks and gowns goes against everything we have been taught as nurses. We do not have the proper PPE needed to protect ourselves and our patients from cross contamination. As direct care providers, we need to be protected and stay healthy so we can continue to care for these patients.”
The previous week, local first responders paid tribute in New Hyde Park to Parker Jewish Institute for Healthcare and Rehabilitation’s front line health care workers battling the pandemic as they finished their shift.
Paying tribute were members of FDNY Engine 251, along with New Hyde Park, Manhasset-Lakeville, Great Neck Alert Fire Company, Bellerose Terrace, Stewart Manor, Garden City Park and South Floral Park Fire Departments. These first responders were joined by members of NYPD 105 Precinct and MTA Police as well as Lake Success, Kings Point, Floral Park and Oyster Bay Cove Police Departments and SeniorCare EMS.
Car caravan
The ‘Parade of Sirens’ was made even more special due to the fact that earlier in the day, Parker released its first recovered COVID-19 patient, James Tully, who doctors said was well enough to return to his Bayside home. Mr. Tully and his family attended the celebration of the staff to thank the them for the care he received in his recovery.
That same week, the Long Island community participated in a car caravan to acknowledge nurses and healthcare workers at Long Island Jewish Valley Stream – Northwell. Among the crowd cheering, honking, and thanking LIJ nurses was State Assemblywoman Michaelle Solages. “It’s important we tell [LIJ healthcare professionals] that we know what you’re doing, to keep up the good fight and to let authorities know that they need more support,” she said.
Fire departments across Long Island are finding creative ways to pay tribute to healthcare workers. The Bethpage Fire Department led a caravan around St. Joseph Hospital on April 16, their cheers and lights bringing reprise to the nurses watching. The Hyde Park Fire Department also led a caravan of trucks and cars from the community to show support for healthcare workers at the Parker Jewish Institute.
The PPE donations, cheers, and caravans from the Long Island community combined in a display of public support.
New York City Health + Hospitals
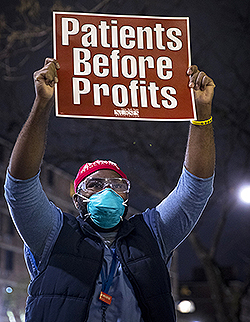
Crossing the 145th Street Bridge that connects Harlem and the South Bronx and continue a few blocks east you find Lincoln Medical Center, one of the busiest hospitals in the NYC Health and Hospitals system.On April 14, nurses gathered in front of Lincoln for a candlelight vigil, an homage to healthcare workers on the front lines in the COVID-19 pandemic. Elsewhere in the Bronx, nurses at Jacobi Medical Center have protested conditions. "Any measures to re-open need to be based on science and fact, not profit and fiction," said Jacobi LBU President Kelley Cabrera, RN.
Diary entries in April from NYC H+H nurses indicated 68 percent lacked adequate PPE. The last week of April that figure dropped to 58 percent. Still, more than half the nurses who forwarded diary entries last month were working with inadequate PPE—still.
One newly active member at a NYC H+H facility drafted a petition with her co-workers for better PPE which resulted in greater compliance with the Governor’s “at least one N95 a day” directive. Another NYC H+H nurse, frustrated with management intimidation, organized fellow nurses to go in groups of twos and threes to sign out their daily N95s. Others did email blitzes to nursing management and HR for fit-testing, organized walk-ins to the command center, and held rallies and press conferences.
Montefiore Medical Center
While the census has come down, hundreds of patients remain critically ill in the ICUs, some of these units are makeshift. At times, ICU nurses are caring for four patients, well beyond the scope of what’s safe. While the peak may be passing, nurses and public health experts warn that a re-opening without a fully staffed hospital runs a serious risk, as a second surge may occur.
“It didn’t have to be this way,” said Rochelle Alexander, a Montefiore Weiler Endoscopy nurse. “We need more staff and resource nurses who can help us. I have the desire to do my best, but I can’t staff the whole floor. Typically the tele nurse has a 5 to 1 ratio. But now we do that some days with an ICU level of care.”
Understaffed ICUs
Alexander has been floating to a new unit every single day. She’s often working in one of the makeshift ICUs that Montefiore hurriedly created.
“Our cup is empty,” she said. “The ratios are still not where they should be. Our frustration is mounting and we need help.”
However, nurse pressure has produced important improvements. “We have fought for daily masks and we get them,” she said. “But there’s a long road ahead.”
Thankfully, the crisis seems to be tapering.
“The COVID admissions are dropping and the ventilator usage is slowing,” she said. But she cautioned against dropping our guard.
“We’re not through this yet,” Alexander said. “We are concerned about a second wind of COVID. If we have not eradicated it fully we will see it again. We want to be hopeful about the treatments and vaccines under research. But we’re still so early in the game. It is a fearful situation. We need to reopen slowly and not feet first.”
Westchester nurses fight on all fronts
In January, the local Rye Brook, NY, economy suffered a blow as the 400-room Doral Arrowwood Hotel closed. But in late March it reopened and its owners have worked with NYSNA to match frontline healthcare workers to its vacant rooms. Nurses who drive long distances to Westchester Medical Center now have a shorter commute. And those who fear infecting their loved ones at home after caring for COVID-19 patients can instead stay at Doral Arrowwood.
Help from the community
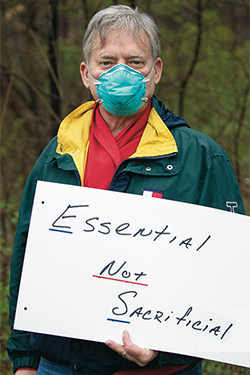
RN Patrice Miloslau, who lives with her 82-year-old mother, signed up for a room through NYSNA. “I’m very appreciative that I have a place to go so my mother will be safe,” she said. “This is a godsend.”Westchester nurses are grateful for help from the community. Still, containing the virus remains an overwhelming task. At Westchester Medical Center, where at one time 20 percent of the facility’s 1,500 RNs were out sick, nurses rallied for more protective gear. “You wouldn’t send a fireman into a fire without his gear,” said David Long, RN. “Don’t send us into this fire without the right gear.”
These sentiments were echoed by nurses at St. John’s Riverside Hospital and St. Joseph’s in Yonkers, which has the highest confirmed number of coronavirus cases in Westchester County. Liya Robin, RN, issued this message to the press: “We want to stay safe, to stay alive, for the future, for today, for our patients.”
Yet Westchester Medical Center continued to fall behind in its provision of PPE to nurses. The mandate by the governor’s COVID-19 Taskforce—that each direct care nurse receive at least one new N95 mask every day—was not being met. That led to NYSNA’s decision to go to court against Westchester Medical Center. Nurses will pursue every route available to them to achieve safety for our colleagues and patients.
Hudson Valley nurses say: follow the science!
On April 20, Health Alliance Hudson Valley nurses spoke out for more protection, more testing, and more effort from the government to solve the COVID-19 pandemic. As one nurse home recovering from COVID said, “Healthcare workers must be routinely tested so they don’t put their colleagues, patients, families and communities at risk.”
“We need clear guidelines with national standard protocols for testing COVID-19 that are based on science, not politics or economics,” she added. Currently, hospitals and state officials continue to remake infection control protocols to fit the shortages of supplies and testing. But RNs know that if they are getting sick, it’s time to raise standards, not lower them.
Albany nurses get results from Governor
It was with a sense of urgency that Albany Medical Center nurses held a speak out in front of their hospital on April 11. After Spectrum News and other outlets reported on Lenore Granich, RN, and her experience of being told to reuse the same N95 mask 20 times, the Governor was asked about it during his daily briefing.
The result was that the state’s COVID-19 Taskforce would set up a line of communication directly with nurses, not just hospital administrations, about sufficiency of PPE and other safety issues in their hospitals. Behind every step the state takes towards fixing the PPE shortage and other matters is a healthcare worker speaking loud and clear about conditions on the frontline.
Buffalo nurses push ECMC in the right direction
On April 2, the Erie County Medical Center nurses rallied alongside the Communications Workers of America to demand adequate supplies of PPE. There was a call on President Trump to invoke the Defense Production Act to mandate production of protective equipment. RN Rachel Larkin asked a powerful question: “So why is it that during wartime, our country can mobilize essentially overnight to mass produce weapons, ammunition, guns, bullets, but during a time when we need to step up and protect our own citizens, we have waited months to even begin to mobilize to produce adequate PPE and ventilators and testing kit supplies?”
NYSNA nurses have asked repeatedly why the Defense Production Act was not invoked to procure and make the equipment desperately needed to shield nurses and treat patients.
ECMC nurses rallied again on April 3 for greater protections against COVID-19. “At times, it has been a struggle to get the PPE and testing we feel is safe and necessary for slowing the spread of COVID-19,” said Steve Bailey, RN. “When we rallied outside the hospital, we were joined in solidarity by ECMC Administration, who committed to get N95s to more nurses. Since then, we have seen them make a good faith effort to protect the nurses on the frontlines.”
Brooklyn nurses highlight disparities
Wyckoff Heights Medical Center in Brooklyn was the first in the city to register a coronavirus-related death. Sadly, that death did not motivate Wyckoff to take action to protect nurses and save patients. A demonstration was organized on April 10 to protest the shortages of PPE, the lack of testing and inadequate staffing impeding their ability to care for their patients.
“You do what needs to be done, but you now have to split your time between four patients. You move from one to the next, it’s almost like an assembly line,” said Coleen Peters, RN. “Sometimes it’s so busy you don’t have time for bathroom breaks or lunch.”
Wyckoff nurses stressed that the inequalities that exist in the community adjacent to the hospital are also affecting the hospital’s resources. Competing for supplies on the open market has left Wyckoff in a losing contest. The voices of nurses at Wyckoff and other safety net facilities must be heard. Any plan for reopening needs to take into consideration our most vulnerable communities, and the healthcare workers that serve them.
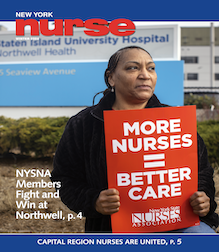
Staten Island nurses stand up to Northwell
Northwell Health, which owns Staten Island University Hospital, is the largest hospital system in New York and the biggest private sector employer in the state. Yet it largely failed to adequately prepare SIUH for COVID-19, even as Staten Island came to have the second-highest concentration of COVID-19 cases in the state.SIUH nurses did not allow Northwell to silence them, holding a speak out about the lack of protective gear and unsafe staffing levels that have put frontline staff and patients in danger. Dawn Cardello, RN, pointed out that Northwell has been pressuring sick nurses to come back to work after only seven days, even if they’re still showing symptoms: “And to add insult to injury,” she said, “Northwell is forcing some nurses to use their own sick time instead of the paid COVID leave, and questioning nurses if they say they’re too sick to come back to work right away.”
Inadequate PPE is linked directly to nurses’ infection rates, a disastrous effect on staffing levels in the hospital. Nurses are taking care of 3 or 4 critical care patients at a time. There is more. “Every day the hospital is changing how they staff different units,” said Cindy Carlin, RN. “They’re sending us to different areas. It’s very choppy, very disorganized, and it has to stop!”
“We’re calling on Northwell CEO Michael Dowling to lead the way,” said Cardello, “and stop lagging behind.” With its size and resources, Northwell sets the tone for the entire state’s response to COVID-19. SIUH nurses are protesting because they know if they can change direction at Northwell, the rest of New York’s hospitals will follow. Nurses are committed to improving their conditions and will not be silenced.
Champlain Valley Physicians Hospital and the Upstate COVID Nurse Corps
The first nurses participating in the Upstate COVID Nurse Corps made their way to NYC on May 4. It was just three weeks ago that Upstate members were first contacted about the Upstate COVID Nurses Corps and more than 120 have volunteered to travel to NYC to assist with the COVID surge.
Champlain Valley Physicians Hospital (CVPH) in Plattsburgh is now partnering with NYSNA to send nurses from Plattsburgh to NYC in phased stages, in a show of solidarity in the fight to stop COVID-19. The first nurses are starting at Richmond University Medical Center (RUMC) on May 5.
“We’ve been preparing for the surge Upstate, but too many nurses are on hold, which makes no sense when people so desperately need help,” said Cassie Stanley, RN.
As part of the Upstate COVID Nurse Corps, Upstate hospitals will guarantee employment and continued health insurance coverage for nurses who volunteer downstate.
“We object to any furloughing...”
In explaining why NYSNA is launching a new program, the Upstate COVID Nurse Corps, Executive Director Pat Kane, RN, said, “Nurses want to do everything they can to slow the spread of COVID-19 and do what they do best — care for patients. We want to make it possible for them to go where the need is greatest.”
Three upstate hospitals serving thousands of patients in the center of the state — St. Elizabeth Medical Center (Mohawk Valley Health System), Albany Medical Center and Nathan Littauer in Gloversville are laying off or furloughing nurses.
“We object to any furloughing or calling off any nurse during a pandemic, because it puts our communities at unnecessary risk,” said NYSNA Board Member Marion Enright, RN of Nathan Littauer Hospital. “We think the Upstate COVID Nurse Corps will be a better alternative and will help our hospitals respond to the COVID crisis in a more unified and effective way.”
NYSNA urged Albany Medical Center to participate in lieu of benching hundreds of nurses, but the Administration declined.
COVID-19 Action Teams
More than 350 members have attended NYSNA’s COVID-19 Action Team trainings since early April.
Around the state seasoned nurse leaders and newly active members join the teams to deal with the dire health and safety, staffing, testing, quarantine, training, and visitation issues of the crisis. Modeled on the Contract Action Team that forms during bargaining, COVID-19 Teams aim for a member on every unit and shift who can quickly circulate health and safety information, coordinate documentation of unsafe conditions, and engage members in collective action to move management. The trainings feature nurse leaders from several facilities who share their CAT fight back stories, presentations from NYSNA health and safety representatives, tips on communication tools and social media, questions and discussion.