Safe nurses, safe communities: the union approach to managing the COVID-19 crisis

UPDATED: March 19, 2020
- Download and distribute the latest NYSNA COVID-19 Update Flier
Providing Care, Often Without Tools We Need
NYSNA members at many facilities are routinely being asked to provide care for patients with confirmed of suspected COVID-19 without proper protection. This includes inadequate respiratory protection and other PPE, inadequate patient care areas, inadequate policies and procedures and inadequate training. Many nurses are being told to reuse respirators in a way that conflicts with manufacturer’s instructions and the CDC’s own infection control guidance.
“We have been down this road before,” one long-time nurse pointed out. “When hazards around bloodborne pathogens soared during the AIDS crisis of the 1980s, we were told that even using gloves was unnecessary. But we fought and won the bloodborne pathogens standard in the OSHA regulations, protecting nurses and other staff going forward.”
NYSNA members should be proud of the work they have been doing in recent years to put healthcare worker safety and health front and center – by taking on rampant workplace violence, challenging chemical exposures, fighting for safe staffing and safe patient handling. Clearly we have a new goal in the coming period: an effective infection control standard adopted by OSHA, the agency that is designated with the role of protecting all workers.
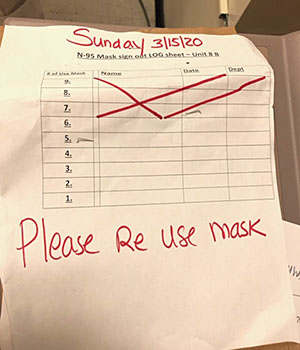
Focus on One Conservation Measure is a Problem
As the clamor grew about a respirator shortage, it became clear that the employers had just one proposed solution: cut back their use at the expense of worker safety. Some have done this by locking up N95s, making it difficult to access them. Others have directed staff to reuse them, storing them in and paper bags between use. All are trying to restrict the care settings in which respirators will be used, including limiting N95 use to only when conducting aerosol-generating procedures.
Largely missing at this time is a multi-system approach that is needed to solve problems in a crisis situation. There are many ways to protect workers and conserve supplies. OSHA, for example, calls for engineering and administrative controls to be used before protective equipment is even considered. See attached list for concrete ideas on what employers can be doing to conserve respirators while still protecting healthcare workers.
NYSNA Workplace Action Plan
- Clear, accurate information is needed to counter the roller coaster of misinformation many of us are experiencing at this time. Phone trees, social media, conference calls and Zoom meetings need to be part of our tool kit going forward. NYSNA is holding regular phone conference calls and virtual town meetings.
- Document and escalate. Which staff have been exposed to COVID-19, which don’t have equipment, what is management saying and doing? This and other real time information is important to share with LBU leadership, NYSNA representatives and NYSNA Health and Safety. File POAs with the COVID-19 amended form found on the NYSNA website.
- Use our right and power to bargain. We have a union and that gives us the right to bargain over changes in working conditions and policies. Now is the time to invoke this right: it may be the only way, in some facilities, to get alternative measures (like those listed below) onto the table.
- “If growing numbers of nurses are not able to be at the bedside because they were exposed to COVID-19 unnecessarily at work, everyone’s health is put in jeopardy. Steps we take now can save lives down the road.” – NYSNA Executive Director Pat Kane
Key Questions on Respiratory Protection
What PPE is needed?
The coronavirus that causes COVID-19 can be transmitted via contact, droplet and airborne routes. NYSNA disagrees with the current position of the CDC, which now states that the virus is primarily transmitted via droplets and, therefore, N95 respirators are only necessary when aerosol-generating procedures are being conducted. At this time it is unclear how frequently transmission takes place via contact and airborne transmission. And of course patient care is subject to sudden and unplanned-for events. Until it is confirmed that healthcare workers are not at risk from contact and/or airborne transmission, NYSNA believes that N95 or higher respirator protection, fluid resistant or impermeable gown, gloves, and face shield or non-vented goggles must be worn by all healthcare workers treating both PUIs (patients under investigation) and confirmed COVID-19 patients.
 Can disposable N95 respirators be safely reused?
Can disposable N95 respirators be safely reused?
There has been much confusion regarding the safe extended use and reuse of disposable respirators. The CDC document entitled Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings (https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html) states that N95 disposable respirators should not be reused if the pathogen in question can be spread via contact or droplets. A disposable N95 can only be reused under very specific circumstances and should not be reused when coming into close contact with COVID-19 suspected or confirmed cases. For more information please review the link above or contact your NYSNA representative.
Manufacturer instructions for use also prohibit the reuse of filtering facepiece respirators. 3M, for eample, states: “When FFRs are used against bioaerosols, they should be discarded after each use, carefully and appropriately, according to local waste disposal guidelines. During use, particles containing viruses, bacteria, etc. get captured on the filter fibers and remain on the fibers. Therefore, after use, handling or storing the respirator might result in further spreading the disease.” —3M Technical Bulletin, February 2020, Revision 3, Respiratory Protection FAQ: Healthcare.
Wise Use of Supplies
Don’t Shortcut Worker Protection; Other Measures Can Conserve PPE
Here are steps that can be taken to insure that respirators and other protective equipment is used wisely during this critical time.
- Organize the assessment and triage of patients suspected of having COVID-19 in order to limit the number of staff exposed. Alternate triage sites, such as trailers or tents, or another part of the hospital, are options. Using and administrative control like this reduces the chance that other staff have to use protective equipment, as it will be limited to staff dedicated to this purpose.
- Organize the care of patients in order to limit the number of staff who may be exposed and thereby reduce the amount of protective equipment needed. This can be done on a large scale, by a city or heath system designating only certain facilities for COVID-19 care. It can be done on the facility level, by designating specific areas, rooms or units and designated care teams for COVID-19 care.
- Expand the supply of N95 respirators by using FDA/NIOSH-approved industrial respirators in addition to surgical N95s. Please note: these respirators are subject to the same fit-testing and medical clearance provisions as surgical N95s. OSHA has recommended this measure.
- Use higher-level respirators that are similar to N95s to extend the supply of N95s. N99 and N100 respirators for example, which are similar to N95s but offer better protection, can be used if N95s are not available. OSHA has recommended this.
- Use higher-level respirators that are not disposable and can be safely reused. Elastomeric half-face respirators can be worn repeatedly provided they are cleaned, disinfected, inspected and repaired properly. Powered air purifying respirators (PAPRs) cover the entire face and supply filtered air to the wearer. These are sometimes used in operating rooms and were required for Ebola care. They can be reused, so supply is far less of an issue. OSHA has recommended this.
- Get supplies of expired N95 respirators to use for annual and new employee fit testing. Fit testing can burn through supplies, especially for large facilities. This will prevent the regular N95s from being used for this purpose. OSHA has approved this.
- Centralize care to certain facilities within healthcare systems. A number of healthcare systems have done this in the past, designating certain facilities for the care of the sickest patients. Given the widespread and rapid increase in COVID-19 patients this may be only possible during certain stages of the crisis – but should be used when feasible.
For further information, questions or concerns, please contact your NYSNA representative.