The crisis within the crisis: COVID-19’s deadly racial disparities

The COVID crisis has laid bare the deep racial inequalities in the nation’s healthcare system, and the consequences of decades of disinvestment in New York’s safety net. Unfortunately, it’s taken months to get most states—and the Centers for Disease Control—to report COVID-19 statistics by race, so we are just beginning to understand the scale this racially disparate impact.
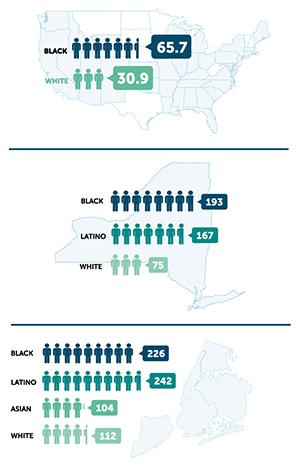
The data paint a sobering picture. As of mid-June, unadjusted COVID-19 death rates for African Americans nationally were twice that whites. In New York, Blacks and Latinos were killed by COVID-19 at two and a half times the rate of whites.
These racial inequalities are even worse when taking account of age differences within the population. For example, according to the latest data from the CDC African Americans between the ages of 35 to 44 were killed by COVID-19 at a rate 10 times higher than their white peers while Latinos in the same age bracket died at a rate 8 times higher than whites.
It’s not biology or “bad habits”
|
Image
|
| Unadjusted COVID-19 Death Rates (per 100,000). Data for the U.S. and New York are taken from the investigative journalism website covidtracking.com, downloaded June 18, 2020. Calculations for the U.S. are based on the 41 states reporting data by race, where fewer than 15 percent of deaths were unclassified. COVID-19 death rates for New York City are calculated based on data from the New York City Department of Health, downloaded on June 18, 2020. |
What’s driving the intense racial disparities with COVID-19?
Whether it’s heart disease or COVID-19, we know there is no genetic or biological basis for racially disparate health outcomes. Indeed, they are a product of a host of other material differences such as access to care, employment, housing, exposure to pollution, and the availability of nutritious, healthy foods.
Collectively, these social determinants of health are the driving force behind observed racial disparities, including many of the comorbidities so commonly viewed as the product of individual choices.
Social determinants of health
One clear example is the fact that African American, Latino, and Asian workers make up a greater proportion of the state’s essential workers. According a recent report from the Center for Economic Policy Research, African Americans made up a third of New York’s public transit workforce and a quarter of the healthcare workforce, while comprising only 14 percent of all workers in the state.
Another factor is that working age African Americans are 50 percent more likely to be uninsured that white New Yorkers. The situation is even worse for Latinos, who are nearly 3 times more likely to be uninsured than white New Yorkers according to the latest Census data.
Housing is another important consideration. In the Bronx, which now has the highest rate of COVID-19 in the state, most people live in apartments, and according to the latest data from New York City, 68 percent of the borough’s apartments have maintenance defects.
Then there are environmental factors. For example, the South Bronx is also home of some of the worst air quality in the country. The neighborhood of Mott Haven is sometimes called “asthma alley” because the high rate of emergency room visits for asthma.
Healthcare policy deprives communities of color
These community-level factors have only been exacerbated by healthcare policy decisions at the state and federal level. For example, New York has shuttered dozens of safety net hospitals across the state in the past 20 years, leaving many of the hardest hit communities without the healthcare infrastructure they needed to care for COVID patients during the surge.
During this same period of time, the state has starved the remaining safety net hospitals of more than $13 billion in funding dedicated to charity care, directing these resources instead to wealthy private hospitals who have very few Medicaid or uninsured patients.
The same pattern can be seen with the distribution of funds from the Federal CARES Act to help New York hospitals handle the surge. Northwell Health, the state’s largest hospital system received $1.1 billion in federal aid, while only 25% of their patients were Medicaid patients. By contrast, the 11 public hospitals that comprise New York City Health and Hospitals, received only $775 million from the CARES Act, despite the fact that 60% of their patients were Medicaid patients.