When the COVID-19 pandemic began, many in the nation developed a deeper appreciation for healthcare workers, including nurses. Even those who long held healthcare workers in high regard became more effusive with praise. Despite years of laboring in a host of difficult circumstances, healthcare workers were suddenly superheroes with capes. In New York City, some people even took to their balconies to clap for those who sacrificed their health to help others. But what nurses truly needed was action from their employers to address staffing shortages.
Understaffing across the board
Nurses at Columbia Presbyterian say staffing ratios have gotten as high as 15 to 1. Nurses in critical care units detail having as many as three and four patients when they should have two. Healthcare workers at Montefiore and other health systems in New York City are sharing similar accounts. The hospital I work for, Maimonides Medical Center in Brooklyn, is down 150 nurses. These shortages are occurring at a time when COVID-19 cases are spiking, which is creating added anxiety. When ratios are high, nurses struggle to meet the individual needs of unique patients, but they also risk physical and emotional harm.
When hospitals fail to staff properly, yet proclaim nurses heroes, they engage in a form of manipulation. While nurses were being publicly praised at the height of the pandemic, they also lacked access to basic Personal Protection Equipment. New York Times columnist Farhad Manjoo agreed:
“A few months ago, it was nurses, doctors and other essential workers who were hailed as heroes — a perfectly accurate and heartwarming sentiment, but also one meant to obscure the sorry reality that the world’s richest country was asking health care workers to treat coronavirus patients without providing adequate protective gear.”
Inaccessible protective equipment coupled with staffing shortages is troublesome mix. Staffing shortages mean co-horting or grouping of patients with similar illnesses, is not happening. Staffing shortages also mean nurses are caring for too many patients of varying acuity levels. Worrisome still, caring for too many patients or working long shifts mean workers are not getting the breaks they need to maintain their own health and wellbeing.
While praise is welcome, it is insufficient to ameliorate what nurses are experiencing. Certainly, there were nursing shortages before the pandemic began, but the pressures of COVID-19 has compounded the situation. Some nurses have left the workforce, others left hospitals for different healthcare settings and others retired early.
“Just in time” means unprepared
As the pandemic has raged on, several lessons are coming into clearer focus. First, in designating health care workers heroes, the lived experience of these workers was masked. In reality, too many healthcare workers were not, and many still are not, receiving the supports they need to do their job. Consequently, many are quitting or refusing to work in hospital settings. This is fueling additional staffing shortages. For those nurses who remain in hospitals, news of the Delta variant is causing many to exclaim, “I can’t go through this again.”
Next, the “just in time” approach adopted by many hospitals promised that healthcare workers would have what they needed “just in time.” But “just in time” creates added strain for already fatigued workers. People on the frontlines should be able to access what they need as soon as they need it. Further, “just in time” models for staffing means institutions are not prepared for emergencies when they do arise.
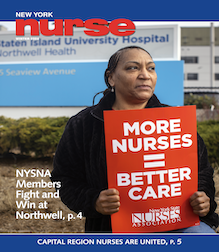
We must push the line
Finally, although unions like ours helped pass New York State Safe Staffing legislation, the law doesn’t go into effect until 2023. It is also a floor and not ceiling for addressing shortages. We must continue to push the line and ensure that workers have what they need to care for themselves, their families and the communities they serve. This means organizing in support of passage of federal legislation, like H.R. 3165 which is pending in Congress. Among other safety precautions, the measure sets minimum nurse-to-patient staffing requirements.
We know that COVID-19 cases are rising. We also know that the DELTA variant poses additional challenges. It is time to address all loopholes that compromise patient care, by jeopardizing the wellbeing of nurses and other healthcare workers. Lip service can only get us so far, and it has yet to save lives.